-
Almazan, F., Gonzalez, J.M., Penzes, Z., Izeta, A., Calvo, E., Plana-Duran, J.,Enjuanes, L., 2000. Engineering the largest RNA virus genome as an infectious bacterial artificial chromosome. Proc. Natl. Acad. Sci. U. S. A., 97, 5516-5521.
-
Bai, Z., Cao, Y., Liu, W.,Li, J., 2021. The SARS-CoV-2 nucleocapsid protein and its role in viral structure, biological functions, and a potential target for drug or vaccine mitigation. Viruses, 13.
-
Bao, L., Deng, W., Huang, B., Gao, H., Liu, J., Ren, L., Wei, Q., Yu, P., Xu, Y., Qi, F., Qu, Y., Li, F., Lv, Q., Wang, W., Xue, J., Gong, S., Liu, M., Wang, G., Wang, S., Song, Z., Zhao, L., Liu, P., Zhao, L., Ye, F., Wang, H., Zhou, W., Zhu, N., Zhen, W., Yu, H., Zhang, X., Guo, L., Chen, L., Wang, C., Wang, Y., Wang, X., Xiao, Y., Sun, Q., Liu, H., Zhu, F., Ma, C., Yan, L., Yang, M., Han, J., Xu, W., Tan, W., Peng, X., Jin, Q., Wu, G.,Qin, C., 2020. The pathogenicity of SARS-CoV-2 in hACE2 transgenic mice. Nature, 583, 830-833.
-
Cai, H.-L.,Huang, Y.-W., 2023. Reverse genetics systems for SARS-CoV-2: development and applications. Virol. Sin., 38, 837-850.
-
Chen, L., Guan, W.J., Qiu, Z.E., Xu, J.B., Bai, X., Hou, X.C., Sun, J., Qu, S., Huang, Z.X., Lei, T.L., Huang, Z.Y., Zhao, J., Zhu, Y.X., Ye, K.N., Lun, Z.R., Zhou, W.L., Zhong, N.S.,Zhang, Y.L., 2022. SARS-CoV-2 nucleocapsid protein triggers hyperinflammation via protein-protein interaction-mediated intracellular Cl(-) accumulation in respiratory epithelium. Signal Transduct. Target. Ther., 7, 255.
-
Chen, Y., Liu, Q.,Guo, D., 2020. Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med. Virol., 92, 418-423.
-
Cheung, P.H., Ye, Z.W., Lui, W.Y., Ong, C.P., Chan, P., Lee, T.T., Tang, T.T., Yuen, T.L., Fung, S.Y., Cheng, Y., Chan, C.P., Chan, C.P.,Jin, D.Y., 2022. Production of single-cycle infectious SARS-CoV-2 through a trans-complemented replicon. J. Med. Virol., 94, 6078-6090.
-
Feng, X., Zhang, X., Jiang, S., Tang, Y., Cheng, C., Krishna, P.A., Wang, X., Dai, J., Zeng, J., Xia, T.,Zhao, D., 2022. A DNA-based non-infectious replicon system to study SARS-CoV-2 RNA synthesis. Comput. Struct. Biotechnol. J., 20, 5193-5202.
-
Hassan, A.O., Case, J.B., Winkler, E.S., Thackray, L.B., Kafai, N.M., Bailey, A.L., Mccune, B.T., Fox, J.M., Chen, R.E., Alsoussi, W.B., Turner, J.S., Schmitz, A.J., Lei, T., Shrihari, S., Keeler, S.P., Fremont, D.H., Greco, S., Mccray, P.B., Jr., Perlman, S., Holtzman, M.J., Ellebedy, A.H.,Diamond, M.S., 2020. A SARS-CoV-2 infection model in mice demonstrates protection by neutralizing antibodies. Cell, 182, 744-753.e744.
-
He, X., Quan, S., Xu, M., Rodriguez, S., Goh, S.L., Wei, J., Fridman, A., Koeplinger, K.A., Carroll, S.S., Grobler, J.A., Espeseth, A.S., Olsen, D.B., Hazuda, D.J.,Wang, D., 2021. Generation of SARS-CoV-2 reporter replicon for high-throughput antiviral screening and testing. Proc. Natl. Acad. Sci. U. S. A., 118.
-
Hou, Y.J., Okuda, K., Edwards, C.E., Martinez, D.R., Asakura, T., Dinnon, K.H., 3rd, Kato, T., Lee, R.E., Yount, B.L., Mascenik, T.M., Chen, G., Olivier, K.N., Ghio, A., Tse, L.V., Leist, S.R., Gralinski, L.E., Schafer, A., Dang, H., Gilmore, R., Nakano, S., Sun, L., Fulcher, M.L., Livraghi-Butrico, A., Nicely, N.I., Cameron, M., Cameron, C., Kelvin, D.J., De Silva, A., Margolis, D.M., Markmann, A., Bartelt, L., Zumwalt, R., Martinez, F.J., Salvatore, S.P., Borczuk, A., Tata, P.R., Sontake, V., Kimple, A., Jaspers, I., O'neal, W.K., Randell, S.H., Boucher, R.C.,Baric, R.S., 2020. SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell, 182, 429-446.e414.
-
Hu, B., Guo, H., Zhou, P.,Shi, Z.L., 2021. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol., 19, 141-154.
-
Jiang, R.D., Liu, M.Q., Chen, Y., Shan, C., Zhou, Y.W., Shen, X.R., Li, Q., Zhang, L., Zhu, Y., Si, H.R., Wang, Q., Min, J., Wang, X., Zhang, W., Li, B., Zhang, H.J., Baric, R.S., Zhou, P., Yang, X.L.,Shi, Z.L., 2020. Pathogenesis of SARS-CoV-2 in transgenic mice expressing human angiotensin-converting enzyme 2. Cell, 182, 50-58.e58.
-
Jin, Y.Y., Lin, H., Cao, L., Wu, W.C., Ji, Y., Du, L., Jiang, Y., Xie, Y., Tong, K., Xing, F., Zheng, F., Shi, M., Pan, J.A., Peng, X.,Guo, D., 2021. A convenient and biosafe replicon with accessory genes of SARS-CoV-2 and its potential application in antiviral drug discovery. Virol. Sin., 36, 913-923.
-
Ju, X., Zhu, Y., Wang, Y., Li, J., Zhang, J., Gong, M., Ren, W., Li, S., Zhong, J., Zhang, L., Zhang, Q.C., Zhang, R.,Ding, Q., 2021. A novel cell culture system modeling the SARS-CoV-2 life cycle. PLoS Pathog., 17, e1009439.
-
Kouprina, N.,Larionov, V., 2006. TAR cloning: insights into gene function, long-range haplotypes and genome structure and evolution. Nat. Rev. Genet., 7, 805-812.
-
Liu, Q., Zhao, H., Li, Z., Zhang, Z., Huang, R., Gu, M., Zhuang, K., Xiong, Q., Chen, X., Yu, W., Qian, S., Zhang, Y., Tan, X., Zhang, M., Yu, F., Guo, M., Huang, Z., Wang, X., Xiang, W., Wu, B., Mei, F., Cai, K., Zhou, L., Zhou, L., Wu, Y., Yan, H., Cao, S., Lan, K.,Chen, Y., 2023. Broadly neutralizing antibodies derived from the earliest COVID-19 convalescents protect mice from SARS-CoV-2 variants challenge. Signal Transduct. Target. Ther., 8, 347.
-
Malicoat, J., Manivasagam, S., Zuniga, S., Sola, I., Mccabe, D., Rong, L., Perlman, S., Enjuanes, L.,Manicassamy, B., 2022. Development of a single-cycle infectious SARS-CoV-2 virus replicon particle system for use in biosafety level 2 laboratories. J. Virol., 96, e0183721.
-
Nguyen, H.T., Falzarano, D., Gerdts, V.,Liu, Q., 2021. Construction of a noninfectious SARS-CoV-2 replicon for antiviral-drug testing and gene function studies. J. Virol., 95, e0068721.
-
Park, S.B., Khan, M., Chiliveri, S.C., Hu, X., Irvin, P., Leek, M., Grieshaber, A., Hu, Z., Jang, E.S., Bax, A.,Liang, T.J., 2023. SARS-CoV-2 omicron variants harbor spike protein mutations responsible for their attenuated fusogenic phenotype. Commun. Biol., 6, 556.
-
Ricardo-Lax, I., Luna, J.M., Thao, T.T.N., Le Pen, J., Yu, Y., Hoffmann, H.H., Schneider, W.M., Razooky, B.S., Fernandez-Martinez, J., Schmidt, F., Weisblum, Y., Trueb, B.S., Berenguer Veiga, I., Schmied, K., Ebert, N., Michailidis, E., Peace, A., Sanchez-Rivera, F.J., Lowe, S.W., Rout, M.P., Hatziioannou, T., Bieniasz, P.D., Poirier, J.T., Macdonald, M.R., Thiel, V.,Rice, C.M., 2021. Replication and single-cycle delivery of SARS-CoV-2 replicons. Science, 374, 1099-1106.
-
Rihn, S.J., Merits, A., Bakshi, S., Turnbull, M.L., Wickenhagen, A., Alexander, A.J.T., Baillie, C., Brennan, B., Brown, F., Brunker, K., Bryden, S.R., Burness, K.A., Carmichael, S., Cole, S.J., Cowton, V.M., Davies, P., Davis, C., De Lorenzo, G., Donald, C.L., Dorward, M., Dunlop, J.I., Elliott, M., Fares, M., Da Silva Filipe, A., Freitas, J.R., Furnon, W., Gestuveo, R.J., Geyer, A., Giesel, D., Goldfarb, D.M., Goodman, N., Gunson, R., Hastie, C.J., Herder, V., Hughes, J., Johnson, C., Johnson, N., Kohl, A., Kerr, K., Leech, H., Lello, L.S., Li, K., Lieber, G., Liu, X., Lingala, R., Loney, C., Mair, D., Mcelwee, M.J., Mcfarlane, S., Nichols, J., Nomikou, K., Orr, A., Orton, R.J., Palmarini, M., Parr, Y.A., Pinto, R.M., Raggett, S., Reid, E., Robertson, D.L., Royle, J., Cameron-Ruiz, N., Shepherd, J.G., Smollett, K., Stewart, D.G., Stewart, M., Sugrue, E., Szemiel, A.M., Taggart, A., Thomson, E.C., Tong, L., Torrie, L.S., Toth, R., Varjak, M., Wang, S., Wilkinson, S.G., Wyatt, P.G., Zusinaite, E., Alessi, D.R., Patel, A.H., Zaid, A., Wilson, S.J.,Mahalingam, S., 2021. A plasmid DNA-launched SARS-CoV-2 reverse genetics system and coronavirus toolkit for COVID-19 research. PLoS Biol., 19, e3001091.
-
Sun, C.P., Jan, J.T., Wang, I.H., Ma, H.H., Ko, H.Y., Wu, P.Y., Kuo, T.J., Liao, H.N., Lan, Y.H., Sie, Z.L., Chen, Y.H., Ko, Y.A., Liao, C.C., Chen, L.Y., Lee, I.J., Tsung, S.I., Lai, Y.J., Chiang, M.T., Liang, J.J., Liu, W.C., Wang, J.R., Yuan, J.P., Lin, Y.S., Tsai, Y.C., Hsieh, S.L., Li, C.W., Wu, H.C., Ko, T.M., Lin, Y.L.,Tao, M.H., 2021. Rapid generation of mouse model for emerging infectious disease with the case of severe COVID-19. PLoS Pathog., 17, e1009758.
-
Takashita, E., Yamayoshi, S., Halfmann, P., Wilson, N., Ries, H., Richardson, A., Bobholz, M., Vuyk, W., Maddox, R., Baker, D.A., Friedrich, T.C., O'connor, D.H., Uraki, R., Ito, M., Sakai-Tagawa, Y., Adachi, E., Saito, M., Koga, M., Tsutsumi, T., Iwatsuki-Horimoto, K., Kiso, M., Yotsuyanagi, H., Watanabe, S., Hasegawa, H., Imai, M.,Kawaoka, Y., 2022. In vitro efficacy of antiviral agents against omicron subvariant BA.4.6. N. Engl. J. Med., 387, 2094-2097.
-
Tanaka, T., Saito, A., Suzuki, T., Miyamoto, Y., Takayama, K., Okamoto, T.,Moriishi, K., 2022. Establishment of a stable SARS-CoV-2 replicon system for application in high-throughput screening. Antiviral Res., 199, 105268.
-
Tang, G., Liu, Z.,Chen, D., 2022. Human coronaviruses: origin, host and receptor. J. Clin. Virol., 155, 105246.
-
Thi Nhu Thao, T., Labroussaa, F., Ebert, N., V'kovski, P., Stalder, H., Portmann, J., Kelly, J., Steiner, S., Holwerda, M., Kratzel, A., Gultom, M., Schmied, K., Laloli, L., Husser, L., Wider, M., Pfaender, S., Hirt, D., Cippa, V., Crespo-Pomar, S., Schroder, S., Muth, D., Niemeyer, D., Corman, V.M., Muller, M.A., Drosten, C., Dijkman, R., Jores, J.,Thiel, V., 2020. Rapid reconstruction of SARS-CoV-2 using a synthetic genomics platform. Nature, 582, 561-565.
-
Thorne, L.G., Bouhaddou, M., Reuschl, A.K., Zuliani-Alvarez, L., Polacco, B., Pelin, A., Batra, J., Whelan, M.V.X., Hosmillo, M., Fossati, A., Ragazzini, R., Jungreis, I., Ummadi, M., Rojc, A., Turner, J., Bischof, M.L., Obernier, K., Braberg, H., Soucheray, M., Richards, A., Chen, K.H., Harjai, B., Memon, D., Hiatt, J., Rosales, R., Mcgovern, B.L., Jahun, A., Fabius, J.M., White, K., Goodfellow, I.G., Takeuchi, Y., Bonfanti, P., Shokat, K., Jura, N., Verba, K., Noursadeghi, M., Beltrao, P., Kellis, M., Swaney, D.L., Garcia-Sastre, A., Jolly, C., Towers, G.J.,Krogan, N.J., 2022. Evolution of enhanced innate immune evasion by SARS-CoV-2. Nature, 602, 487-495.
-
Wang, B., Zhang, C., Lei, X., Ren, L., Zhao, Z., Wang, J.,Huang, H., 2021. Construction of non-infectious SARS-CoV-2 replicons and their application in drug evaluation. Virol. Sin., 36, 890-900.
-
Wang, W., Peng, X., Jin, Y., Pan, J.A.,Guo, D., 2022. Reverse genetics systems for SARS-CoV-2. J. Med. Virol., 94, 3017-3031.
-
Winkler, E.S., Bailey, A.L., Kafai, N.M., Nair, S., Mccune, B.T., Yu, J., Fox, J.M., Chen, R.E., Earnest, J.T., Keeler, S.P., Ritter, J.H., Kang, L.I., Dort, S., Robichaud, A., Head, R., Holtzman, M.J.,Diamond, M.S., 2020. SARS-CoV-2 infection of human ACE2-transgenic mice causes severe lung inflammation and impaired function. Nat. Immunol., 21, 1327-1335.
-
Wu, A., Peng, Y., Huang, B., Ding, X., Wang, X., Niu, P., Meng, J., Zhu, Z., Zhang, Z., Wang, J., Sheng, J., Quan, L., Xia, Z., Tan, W., Cheng, G.,Jiang, T., 2020. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe, 27, 325-328.
-
Xie, X., Muruato, A., Lokugamage, K.G., Narayanan, K., Zhang, X., Zou, J., Liu, J., Schindewolf, C., Bopp, N.E., Aguilar, P.V., Plante, K.S., Weaver, S.C., Makino, S., Leduc, J.W., Menachery, V.D.,Shi, P.Y., 2020. An infectious cDNA clone of SARS-CoV-2. Cell Host Microbe, 27, 841-848.e843.
-
Yang, B., Liu, C., Ju, X., Wu, B., Wang, Z., Dong, F., Yu, Y., Hou, X., Fang, M., Gao, F., Guo, X., Gui, Y., Ding, Q.,Li, W., 2023. A tissue specific-infection mouse model of SARS-CoV-2. Cell Discov., 9, 43.
-
Ye, C., Chiem, K., Park, J.G., Oladunni, F., Platt, R.N., 2nd, Anderson, T., Almazan, F., De La Torre, J.C.,Martinez-Sobrido, L., 2020. Rescue of SARS-CoV-2 from a single bacterial artificial chromosome. mBio, 11.
-
Zhang, H., Fischer, D.K., Shuda, M., Moore, P.S., Gao, S.J., Ambrose, Z.,Guo, H., 2022. Construction and characterization of two SARS-CoV-2 minigenome replicon systems. J. Med. Virol., 94, 2438-2452.
-
Zhang, X., Liu, Y., Liu, J., Bailey, A.L., Plante, K.S., Plante, J.A., Zou, J., Xia, H., Bopp, N.E., Aguilar, P.V., Ren, P., Menachery, V.D., Diamond, M.S., Weaver, S.C., Xie, X.,Shi, P.Y., 2021. A trans-complementation system for SARS-CoV-2 recapitulates authentic viral replication without virulence. Cell, 184, 2229-2238.e2213.
-
Zhang, Y., Song, W., Chen, S., Yuan, Z.,Yi, Z., 2021. A bacterial artificial chromosome (BAC)-vectored noninfectious replicon of SARS-CoV-2. Antiviral Res., 185, 104974.
-
Zhang, Z.Y., Ju, C.Y., Wu, L.Z., Yan, H., Hong, W.B., Chen, H.Z., Yang, P.B., Wang, B.R., Gou, T., Chen, X.Y., Jiang, Z.H., Wang, W.J., Lin, T., Li, F.N.,Wu, Q., 2023. Therapeutic potency of compound RMY-205 for pulmonary fibrosis induced by SARS-CoV-2 nucleocapsid protein. Cell Chem. Biol., 30, 261-277.e268.
-
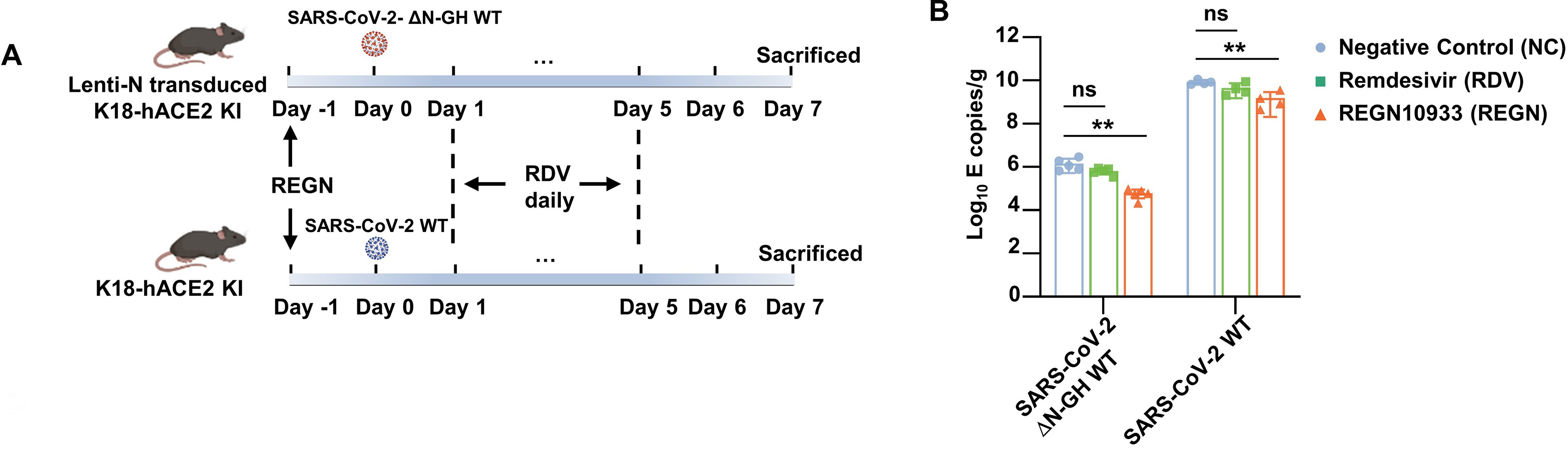
Zheng, J., Wong, L.R., Li, K., Verma, A.K., Ortiz, M.E., Wohlford-Lenane, C., Leidinger, M.R., Knudson, C.M., Meyerholz, D.K., Mccray, P.B., Jr.,Perlman, S., 2021. COVID-19 treatments and pathogenesis including anosmia in K18-hACE2 mice. Nature, 589, 603-607.











 DownLoad:
DownLoad: