-
Banadyga, L., Dolan, M.A., Ebihara, H., 2016. Rodent-adapted filoviruses and the Molecular basis of pathogenesis. J. Mol. Biol. 428, 3449-3466.
-
Baseler, L., Chertow, D.S., Johnson, K.M., Feldmann, H., Morens, D.M., 2017. The pathogenesis of ebola virus disease. Annual review of pathology 12, 387-418.
-
Beier, K.T., Saunders, A., Oldenburg, I.A., Miyamichi, K., Akhtar, N., Luo, L., Whelan, S.P., Sabatini, B., Cepko, C.L., 2011. Anterograde or retrograde transsynaptic labeling of CNS neurons with vesicular stomatitis virus vectors. Proc. Natl. Acad. Sci. U.S.A. 108, 15414-15419.
-
Beier, K.T., Saunders, A.B., Oldenburg, I.A., Sabatini, B.L., Cepko, C.L., 2013. Vesicular stomatitis virus with the rabies virus glycoprotein directs retrograde transsynaptic transport among neurons in vivo. Front. Neural Circ. 7, 11.
-
Benonisson, H., Altintas, I., Sluijter, M., Verploegen, S., Labrijn, A.F., Schuurhuis, D.H., Houtkamp, M.A., Verbeek, J.S., Schuurman, J., van Hall, T., 2019. CD3-Bispecific antibody therapy Turns Solid tumors into inflammatory Sites but Does not Install protective memory. Mol. Cancer Therapeut. 18, 312-322.
-
Bente, D., Gren, J., Strong, J.E., Feldmann, H., 2009. Disease modeling for ebola and marburg viruses. Disease models & mechanisms 2, 12-17.
-
Bowen, E.T., Lloyd, G., Harris, W.J., Platt, G.S., Baskerville, A., Vella, E.E., 1977. Viral haemorrhagic fever in southern Sudan and northern Zaire. Preliminary studies on the aetiological agent. Lancet (London, England) 1, 571-573.
-
Bowen, E.T., Platt, G.S., Simpson, D.I., McArdell, L.B., Raymond, R.T., 1978. Ebola haemorrhagic fever: experimental infection of monkeys. Trans. R. Soc. Trop. Med. Hyg. 72, 188-191.
-
Bradfute, S.B., Swanson, P.E., Smith, M.A., Watanabe, E., McDunn, J.E., Hotchkiss, R.S., Bavari, S., 2010. Mechanisms and consequences of ebolavirus-induced lymphocyte apoptosis. J. Immunol. (Baltimore, Md. 1950) 184, 327-335.
-
Bradfute, S.B., Warfield, K.L., Bray, M., 2012. Mouse models for filovirus infections. Viruses 4, 1477-1508.
-
Brasel, T., Comer, J.E., Massey, S., Smith, J., Smith, J., Hyde, M., Kocsis, A., Gainey, M., Niemuth, N., Triplett, C., Rudge, T., Jr., 2021. Mucosal challenge ferret models of ebola virus disease. Pathogens 10, 292.
-
Bray, M., 2001. The role of the Type I interferon response in the resistance of mice to filovirus infection. J. Gen. Virol. 82, 1365-1373.
-
Bray, M., Davis, K., Geisbert, T., Schmaljohn, C., Huggins, J., 1999. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis. 179 Suppl. 1, S248-S258.
-
Bukreyev, A., Marzi, A., Feldmann, F., Zhang, L., Yang, L., Ward, J.M., Dorward, D.W., Pickles, R.J., Murphy, B.R., Feldmann, H., Collins, P.L., 2009. Chimeric human parainfluenza virus bearing the Ebola virus glycoprotein as the sole surface protein is immunogenic and highly protective against Ebola virus challenge. Virology 383, 348-361.
-
Coltart, C.E., Lindsey, B., Ghinai, I., Johnson, A.M., Heymann, D.L., 2017. The Ebola outbreak, 2013-2016: old lessons for new epidemics. Phil. Trans. Roy. Soc. Lond. B Biol. Sci. 372, 20160297.
-
Connolly, B.M., Steele, K.E., Davis, K.J., Geisbert, T.W., Kell, W.M., Jaax, N.K., Jahrling, P.B., 1999. Pathogenesis of experimental Ebola virus infection in Guinea pigs. J. Infect. Dis. 179 Suppl. 1, S203-S217.
-
Cooper, T.K., Huzella, L., Johnson, J.C., Rojas, O., Yellayi, S., Sun, M.G., Bavari, S., Bonilla, A., Hart, R., Jahrling, P.B., Kuhn, J.H., Zeng, X., 2018. Histology, immunohistochemistry, and in situ hybridization reveal overlooked Ebola virus target tissues in the Ebola virus disease Guinea pig model. Sci. Rep. 8, 1250.
-
Cross, R.W., Mire, C.E., Borisevich, V., Geisbert, J.B., Fenton, K.A., Geisbert, T.W., 2016. The domestic ferret (Mustela putorius furo) as a lethal infection model for 3 species of ebolavirus. J. Infect. Dis. 214, 565-569.
-
Ebihara, H., Rockx, B., Marzi, A., Feldmann, F., Haddock, E., Brining, D., LaCasse, R.A., Gardner, D., Feldmann, H., 2011. Host response dynamics following lethal infection of rhesus macaques with Zaire ebolavirus. J. Infect. Dis. 204 Suppl. 3, S991-S999.
-
Ebihara, H., Takada, A., Kobasa, D., Jones, S., Neumann, G., Theriault, S., Bray, M., Feldmann, H., Kawaoka, Y., 2006. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog. 2, e73.
-
Ebihara, H., Zivcec, M., Gardner, D., Falzarano, D., LaCasse, R., Rosenke, R., Long, D., Haddock, E., Fischer, E., Kawaoka, Y., Feldmann, H., 2013. A Syrian golden hamster model recapitulating ebola hemorrhagic fever. J. Infect. Dis. 207, 306-318.
-
Feldmann, H., Sprecher, A., Geisbert, T.W., 2020. Ebola. N. Engl. J. Med. 382, 1832-1842.
-
Fultz, P.N., Holland, J.J., 1985. Differing responses of hamsters to infection by vesicular stomatitis virus Indiana and New Jersey serotypes. Virus Res. 3, 129-140.
-
Fultz, P.N., Shadduck, J.A., Kang, C.Y., Streilein, J.W., 1981. Genetic analysis of resistance to lethal infections of vesicular stomatitis virus in Syrian hamsters. Infect. Immun. 32, 1007-1013.
-
Garbutt, M., Liebscher, R., Wahl-Jensen, V., Jones, S., Moller, P., Wagner, R., Volchkov, V., Klenk, H.D., Feldmann, H., Stroher, U., 2004. Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J. Virol. 78, 5458-5465.
-
Geisbert, T.W., Feldmann, H., 2011. Recombinant vesicular stomatitis virus-based vaccines against Ebola and Marburg virus infections. J. Infect. Dis. 204 Suppl. 3, S1075-S1081.
-
Geisbert, T.W., Pushko, P., Anderson, K., Smith, J., Davis, K.J., Jahrling, P.B., 2002. Evaluation in nonhuman primates of vaccines against Ebola virus. Emerg. Infect. Dis. 8, 503-507.
-
Glaze, E.R., Roy, M.J., Dalrymple, L.W., Lanning, L.L., 2015. A comparison of the pathogenesis of marburg virus disease in humans and nonhuman primates and evaluation of the suitability of these animal models for predicting clinical efficacy under the 'animal rule'. Comp. Med. 65, 241-259.
-
Jacob, S.T., Crozier, I., Fischer, W.A., Hewlett, A., Kraft, C.S., Vega, M.A., Soka, M.J., Wahl, V., Griffiths, A., Bollinger, L., Kuhn, J.H., 2020. Ebola virus disease. Nat. Rev. Dis. Prim. 6, 13.
-
Johnson, D.M., Brasel, T., Massey, S., Smith, J., Garron, T., Wallace, S., Yu, X., Beasley, D.W., Comer, J.E., 2023. Characterization of ebola virus mucosal challenge routes in cynomolgus macaques. J. Virol. 97, e0188822.
-
Keck, Z.Y., Enterlein, S.G., Howell, K.A., Vu, H., Shulenin, S., Warfield, K.L., Froude, J.W., Araghi, N., Douglas, R., Biggins, J., Lear-Rooney, C.M., Wirchnianski, A.S., Lau, P., Wang, Y., Herbert, A.S., Dye, J.M., Glass, P.J., Holtsberg, F.W., Foung, S.K., Aman, M.J., 2016. Macaque monoclonal antibodies targeting novel conserved epitopes within filovirus glycoprotein. J. Virol. 90, 279-291.
-
Kozak, R., He, S., Kroeker, A., de La Vega, M.A., Audet, J., Wong, G., Urfano, C., Antonation, K., Embury-Hyatt, C., Kobinger, G.P., Qiu, X., 2016. Ferrets infected with bundibugyo virus or ebola virus recapitulate important aspects of human filovirus disease. J. Virol. 90, 9209-9223.
-
Lawson, N.D., Stillman, E.A., Whitt, M.A., Rose, J.K., 1995. Recombinant vesicular stomatitis viruses from DNA. Proc. Natl. Acad. Sci. U.S.A. 92, 4477-4481.
-
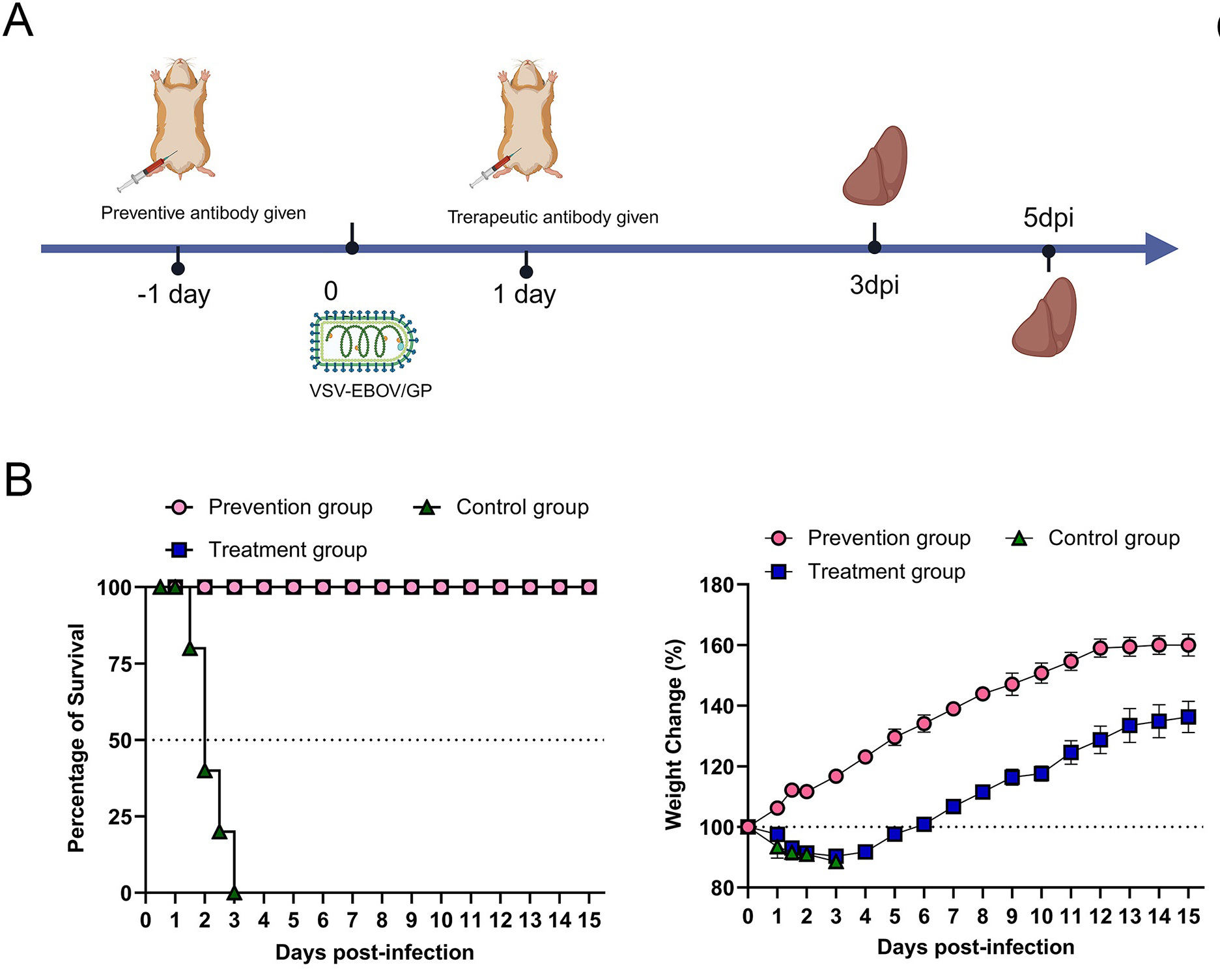
Lee, H.N., McWilliams, I.L., Lewkowicz, A.P., Engel, K., Ireland, D.D.C., Kelley-Baker, L., Thacker, S., Piccardo, P., Manangeeswaran, M., Verthelyi, D., 2021. Characterization of the therapeutic effect of antibodies targeting the Ebola glycoprotein using a novel BSL2-compliant rVSVΔG-EBOV-GP infection model. Emerg. Microb. Infect. 10, 2076-2089.
-
Leligdowicz, A., Fischer, W.A., Uyeki, T.M., Fletcher, T.E., Adhikari, N.K., Portella, G., Lamontagne, F., Clement, C., Jacob, S.T., Rubinson, L., Vanderschuren, A., Hajek, J., Murthy, S., Ferri, M., Crozier, I., Ibrahima, E., Lamah, M.C., Schieffelin, J.S., Brett-Major, D., Bausch, D.G., Shindo, N., Chan, A.K., O'Dempsey, T., Mishra, S., Jacobs, M., Dickson, S., Lyon, G.M., Fowler, R.A., 2016. Ebola virus disease and critical illness. Crit. Care 20, 217.
-
Liu, D.X., Pahar, B., Cooper, T.K., Perry, D.L., Xu, H., Huzella, L.M., Adams, R.D., Hischak, A.M.W., Hart, R.J., Bernbaum, R., Rivera, D., Anthony, S., Claire, M.S., Byrum, R., Cooper, K., Reeder, R., Kurtz, J., Hadley, K., Wada, J., Crozier, I., Worwa, G., Bennett, R.S., Warren, T., Holbrook, M.R., Schmaljohn, C.S., Hensley, L.E., 2023. Ebola virus disease features hemophagocytic lymphohistiocytosis/macrophage activation syndrome in the rhesus macaque model. J. Infect. Dis. 228, 371-382.
-
Manangeeswaran, M., Ireland, D.D., Verthelyi, D., 2016. Zika (PRVABC59) infection is associated with T cell infiltration and neurodegeneration in CNS of immunocompetent neonatal C57Bl/6 mice. PLoS Pathog. 12, e1006004.
-
Martin, B., Canard, B., Decroly, E., 2017. Filovirus proteins for antiviral drug discovery: structure/function bases of the replication cycle. Antivir. Res. 141, 48-61.
-
Martin, B., Hoenen, T., Canard, B., Decroly, E., 2016. Filovirus proteins for antiviral drug discovery: a structure/function analysis of surface glycoproteins and virus entry. Antivir. Res. 135, 1-14.
-
McWilliams, I.L., Kielczewski, J.L., Ireland, D.D.C., Sykes, J.S., Lewkowicz, A.P., Konduru, K., Xu, B.C., Chan, C.C., Caspi, R.R., Manangeeswaran, M., Verthelyi, D., 2019. Pseudovirus rVSVΔG-ZEBOV-GP infects neurons in retina and CNS, causing apoptosis and neurodegeneration in neonatal mice. Cell Rep. 26, 1718-1726.e1714.
-
Muik, A., Stubbert, L.J., Jahedi, R.Z., Geiβ, Y., Kimpel, J., Dold, C., Tober, R., Volk, A., Klein, S., Dietrich, U., Yadollahi, B., Falls, T., Miletic, H., Stojdl, D., Bell, J.C., von Laer, D., 2014. Re-engineering vesicular stomatitis virus to abrogate neurotoxicity, circumvent humoral immunity, and enhance oncolytic potency. Cancer Res. 74, 3567-3578.
-
Nakayama, E., Saijo, M., 2013. Animal models for Ebola and Marburg virus infections. Front. Microbiol. 4, 267.
-
Nicastri, E., Kobinger, G., Vairo, F., Montaldo, C., Mboera, L.E.G., Ansunama, R., Zumla, A., Ippolito, G., 2019. Ebola virus disease: epidemiology, clinical features, management, and prevention. Infect. Dis. Clin. 33, 953-976.
-
Ryabchikova, E., Kolesnikova, L., Smolina, M., Tkachev, V., Pereboeva, L., Baranova, S., Grazhdantseva, A., Rassadkin, Y., 1996. Ebola virus infection in Guinea pigs: presumable role of granulomatous inflammation in pathogenesis. Arch. Virol. 141, 909-921.
-
Shantha, J.G., Crozier, I., Hayek, B.R., Bruce, B.B., Gargu, C., Brown, J., Fankhauser, J., Yeh, S., 2017. Ophthalmic manifestations and causes of vision impairment in ebola virus disease survivors in monrovia, Liberia. Ophthalmology 124, 170-177.
-
Simpson, D.I., Zlotnik, I., Rutter, D.A., 1968. Vervet monkey disease. Experiment infection of Guinea pigs and monkeys with the causative agent. Br. J. Exp. Pathol. 49, 458-464.
-
Siragam, V., Wong, G., Qiu, X.G., 2018. Animal models for filovirus infections. Zool. Res. 39, 15-24.
-
St Claire, M.C., Ragland, D.R., Bollinger, L., Jahrling, P.B., 2017. Animal models of ebolavirus infection. Comp. Med. 67, 253-262.
-
Subbotina, E., Dadaeva, A., Kachko, A., Chepurnov, A., 2010. Genetic factors of Ebola virus virulence in Guinea pigs. Virus Res. 153, 121-133.
-
Wahl-Jensen, V., Bollinger, L., Safronetz, D., de Kok-Mercado, F., Scott, D.P., Ebihara, H., 2012. Use of the Syrian hamster as a new model of ebola virus disease and other viral hemorrhagic fevers. Viruses 4, 3754-3784.
-
Wang, H., Wong, G., Zhu, W., He, S., Zhao, Y., Yan, F., Rahim, M.N., Bi, Y., Zhang, Z., Cheng, K., Jin, H., Cao, Z., Zheng, X., Gai, W., Bai, J., Chen, W., Zou, Y., Gao, Y., Gao, G.F., Yang, S., Xia, X., Qiu, X., 2019. Equine-origin immunoglobulin fragments protect nonhuman primates from ebola virus disease. J. Virol. 93, e01548-18.
-
Wang, S., Liang, B., Wang, W., Li, L., Feng, N., Zhao, Y., Wang, T., Yan, F., Yang, S., Xia, X., 2023. Viral vectored vaccines: design, development, preventive and therapeutic applications in human diseases. Signal Transduct. Targeted Ther. 8, 149.
-
Wang, S., Zhang, C., Liang, B., Wang, W., Feng, N., Zhao, Y., Wang, T., Guo, Z., Yan, F., Yang, S., Xia, X., 2022. Characterization of immune response diversity in rodents vaccinated with a vesicular stomatitis virus vectored COVID-19 vaccine. Viruses 14, 1127.
-
Warfield, K.L., Bradfute, S.B., Wells, J., Lofts, L., Cooper, M.T., Alves, D.A., Reed, D.K., VanTongeren, S.A., Mech, C.A., Bavari, S., 2009. Development and characterization of a mouse model for Marburg hemorrhagic fever. J. Virol. 83, 6404-6415.
-
Warren, T., Zumbrun, E., Weidner, J.M., Gomba, L., Rossi, F., Bannister, R., Tarrant, J., Reed, M., Lee, E., Raymond, J.L., Wells, J., Shamblin, J., Wetzel, K., Donnelly, G., Van Tongeren, S., Lackemeyer, N., Steffens, J., Kimmel, A., Garvey, C., Bloomfield, H., Blair, C., Singh, B., Bavari, S., Cihlar, T., Porter, D., 2020. Characterization of ebola virus disease (EVD) in rhesus monkeys for development of EVD therapeutics. Viruses 12, 92.
-
Wollmann, G., Drokhlyansky, E., Davis, J.N., Cepko, C., van den Pol, A.N., 2015. Lassa-vesicular stomatitis chimeric virus safely destroys brain tumors. J. Virol. 89, 6711-6724.
-
Wong, G., Leung, A., He, S., Cao, W., De La Vega, M.A., Griffin, B.D., Soule, G., Kobinger, G.P., Kobasa, D., Qiu, X., 2018. The makona variant of ebola virus is highly lethal to immunocompromised mice and immunocompetent ferrets. J. Infect. Dis. 218, S466-s470.
-
Woolsey, C., Fears, A.C., Borisevich, V., Agans, K.N., Dobias, N.S., Prasad, A.N., Deer, D.J., Geisbert, J.B., Fenton, K.A., Geisbert, T.W., Cross, R.W., 2022. Natural history of Sudan ebolavirus infection in rhesus and cynomolgus macaques. Emerg. Microb. Infect. 11, 1635-1646.
-
Xie, P., Zhang, M., He, S., Lu, K., Chen, Y., Xing, G., Lu, Y., Liu, P., Li, Y., Wang, S., Chai, N., Wu, J., Deng, H., Wang, H.R., Cao, Y., Zhao, F., Cui, Y., Wang, J., He, F., Zhang, L., 2014. The covalent modifier Nedd8 is critical for the activation of Smurf1 ubiquitin ligase in tumorigenesis. Nat. Commun. 5, 3733.
-
Yan, F., He, S., Banadyga, L., Zhu, W., Zhang, H., Rahim, M.N., Collignon, B., Senthilkumaran, C., Embury-Hyatt, C., Qiu, X., 2019. Characterization of Reston virus infection in ferrets. Antivir. Res. 165, 1-10.
-
Zumbrun, E.E., Bloomfield, H.A., Dye, J.M., Hunter, T.C., Dabisch, P.A., Garza, N.L., Bramel, N.R., Baker, R.J., Williams, R.D., Nichols, D.K., Nalca, A., 2012. A characterization of aerosolized Sudan virus infection in African green monkeys, cynomolgus macaques, and rhesus macaques. Viruses 4, 2115-2136.









 DownLoad:
DownLoad: